Scientists reveal that neurodegenerative diseases aren’t caused by rogue genes, but by the brain’s failing cleanup systems—offering new hope for early detection and treatment.
 Study: The genetics of neurodegenerative diseases is the genetics of age-related damage clearance failure. Image Credit: Kateryna Kon / Shutterstock
Study: The genetics of neurodegenerative diseases is the genetics of age-related damage clearance failure. Image Credit: Kateryna Kon / Shutterstock
Did you know that neurodegenerative diseases, including Alzheimer’s and Parkinson’s, primarily result from failures in clearing damaged proteins? In a recent review published in the journal Molecular Psychiatry, researchers explored how genetic variations affect the body's ability to remove harmful protein accumulations. The findings indicated that these diseases stem from declining clearance mechanisms rather than direct genetic mutations, and suggested new strategies for diagnosis and treatment.
Toxic Protein Accumulation
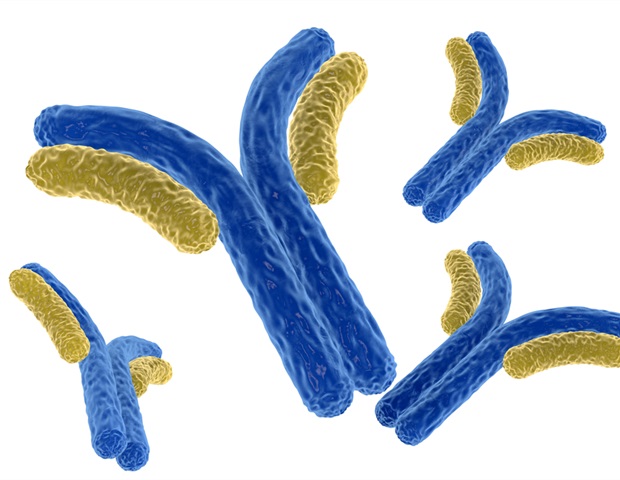
Neurodegenerative diseases, such as Alzheimer’s and Parkinson’s, arise from progressive damage to brain cells, often linked to protein accumulation. Normally, the body has efficient clearance systems, including microglia, lysosomes, and the ubiquitin-proteasome pathway, to remove misfolded or excess proteins. However, as individuals age, these mechanisms weaken, leading to the accumulation of toxic proteins like amyloid-beta, tau, and alpha-synuclein.
Genetic research has identified several risk factors, but most associated genes are involved in clearance pathways rather than directly causing disease. Studies suggest that variations in these genes reduce the efficiency of protein removal, increasing disease risk. Additionally, many patients exhibit multiple overlapping pathologies, complicating diagnosis and treatment.
Genetic Basis of Protein Accumulation
The review explored why specific proteins accumulate in neurodegenerative diseases and discussed existing research that indicates that proteins such as amyloid-beta, tau, and alpha-synuclein originate from highly expressed genes and accumulate when clearance mechanisms falter. Genetic factors, including gene duplications (e.g., APP, SNCA, MAPT) and variations in protein synthesis regulation (such as through antisense transcripts or pseudogenes), contribute to disease risk. However, late-onset cases are more influenced by reduced protein clearance than increased production of these proteins, particularly in Alzheimer’s disease.
Co-pathologies, where multiple neurodegenerative markers coexist, were also found to be common in elderly individuals. Amyloid plaques, tau tangles, and Lewy bodies frequently appear together in elderly patients, suggesting interconnected clearance pathways. The researchers discussed how spillover from one failing clearance pathway to another can overload other pathways, leading to multiple deposits. For example, the failure of the tau clearance pathway in the medial temporal lobe (a condition known as Primary Age-Related Tauopathy or PART) may allow amyloid deposition to spread tangle pathology to the cortex. However, they observed that no direct causal links between different protein accumulations have been definitively established.
Furthermore, certain genetic loci are associated with multiple neurodegenerative conditions, such as mutations in the gene encoding Leucine-Rich Repeat Kinase 2 (LRRK2), which can lead to either Parkinson’s disease with Lewy bodies or tauopathy. This suggested that genetic variations influence how the body responds to cellular damage rather than directly determining pathology.
Additionally, the review discussed the role of incomplete penetrance in near-Mendelian mutations, explaining that incomplete penetrance likely reflects age-related declines in clearance capacity and environmental factors. While some individuals with high-risk mutations remain unaffected, others develop severe symptoms, likely due to additional genetic or environmental influences.
Moreover, the researchers reported that age dependency in neurodegenerative diseases is linked to declining protein clearance efficiency. While genetic risk factors are present from birth, these diseases typically manifest later in life as clearance mechanisms weaken with age. This supported the idea that aging itself is a primary driver of neurodegeneration, emphasizing the need for therapies targeting age-related clearance failures.
Impaired Clearance Systems
The study also indicated that genetic risk is not static but shifts across an individual’s lifespan, with some risk variants having stronger effects at specific ages. For example, the APOE4 allele, which has the largest effect on Alzheimer’s risk, shows changing allele frequencies and odds ratios with age. Given that these diseases significantly contribute to mortality, the researchers stated that their genetic architecture must be analyzed in age-specific contexts to improve predictive accuracy.
The review also examined genome-wide association studies (GWAS), which have been instrumental in identifying genetic risk factors. However, it found that existing datasets often lack age-matched analyses. Most Alzheimer’s disease GWAS are based on dementia diagnoses rather than confirmed pathological markers, which complicates the interpretation of findings.
Furthermore, the researchers underscored the urgent need for genetic studies in non-European populations. Current findings are primarily derived from Northern European cohorts, limiting their applicability to diverse genetic backgrounds. The few studies conducted among African and Asian populations have already revealed differences in risk variants, such as the ABCA7 internally deleted allele in African Americans and the GBA-PD allele in African-derived populations, highlighting the necessity of broadening research efforts.
Additionally, the researchers believe future studies should integrate genetic, biomarker, and imaging data to identify high-risk individuals before clinical symptoms appear. They specifically recommended GWAS of age-specific risks, pathology-confirmed cases, disease progression rates, and analyses of quantitative biomarkers like AB peptides, GFAP, NFL, and p-Tau. Targeted interventions to slow or prevent disease onset can be developed by analyzing disease progression rates and age-specific genetic effects. The review emphasized that advancing precision medicine approaches will require moving beyond broad case-control studies to more nuanced analyses incorporating genetic and biomarker interactions over time.

Cartoon suggesting the possible relationships between the different disease pathologies: amyloid, cleared largely by the microglia; tau, clearly largely by the ubiquitin-proteasome and synuclein, cleared mainly through the lysosome.
Conclusions
To summarize, the study reinforced the concept that neurodegenerative diseases result primarily from failures in protein clearance rather than direct genetic mutations. Age-related declines in clearance capacity play a crucial role, making late-onset diseases an inevitable consequence of aging.
The findings suggested that future research should prioritize age-specific genetic analyses, biomarker integration, and diverse population studies to refine diagnostic tools and develop targeted therapies. Addressing protein clearance failures may be the key to delaying or preventing neurodegenerative disorders.
Journal reference:
- Hardy, J., & Escott-Price, V. (2025). The genetics of neurodegenerative diseases are the genetics of age-related damage clearance failure. Molecular Psychiatry. DOI:10.1038/s41380-025-02911-7, https://www.nature.com/articles/s41380-025-02911-7

 4 hours ago
1
4 hours ago
1














.png)

.png)
.png)
.png)













 English (US) ·
English (US) ·  Hindi (IN) ·
Hindi (IN) ·