Ijeoma Uchegbu, Professor of Pharmaceutical Nanoscience at UCL and Co-Founder and CSO of Nanomerics, gave one of this year's keynote presentations at ELRIG Drug Discovery 2024 in London. ELRIG Drug Discovery is Europe's largest conference for the drug discovery community, providing attendees with the thought and industry leaders at the forefront of drug discovery. In her address, Ijeoma Uchegbu showcased how nanoparticles can be used to improve medication adherence, as well as a novel non-addictive pain product that has the potential to address the opioid crisis.
Why aren’t patients taking their medication, and why that’s a problem for people in drug discovery and drug delivery?
Research shows that patients with chronic conditions often don’t take their medications as prescribed. They may miss doses or stop entirely. In the U.S., financial reasons are a big issue. Also, there’s the issue of side effects. These aren’t life-limiting or particularly lifestyle-limiting, but they’re uncomfortable and inconvenient. For example, someone who’s had a stroke and is likely to have a second one might stop taking medication due to nausea or stomach upset, which increases their risk of stroke. So, side effects, which seem mild, can actually have a large impact.

Image Credit: ELRIG UK
There’s also a group of patients who don’t believe in medication. Social scientists and pharmacists can educate them, but if their resistance is rooted in something pharmacological, counseling may not change adherence. Sometimes, a drug hits a receptor in an unintended area, causing side effects. If we can direct the drug away from these tissues, we have a chance to reduce those effects.
How do nanoparticles and nanomedicine impact the problem of people not taking their medication?
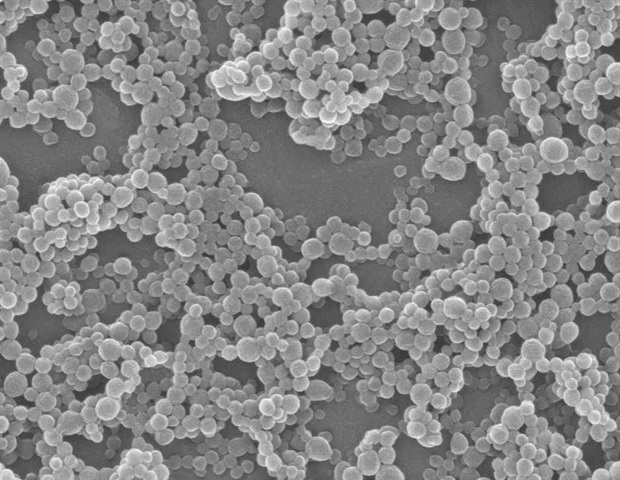
Take eye drops as an example. Preclinically, we’ve shown that we can deliver them to the retina. If a patient has injections into the eye, they might try to skip one, deteriorating their condition. Eye drops, while not easy, are still simpler than injections, so if patients can use eye drops at home, they’re more likely to take their medication.
For example, eye drops may deliver some drugs into the blood, which can cause side effects. With our nanoparticles, most of the drug goes into the tissues, and we don’t detect it in the blood. This control lets us lower the dose and reduce side effects.
How did the molecule leucine enkephalin inspire the development of Envelta, a non-addictive pain product?
Leucine enkephalin is released during painful stimuli and has a short half-life, allowing it to be released again quickly. These molecules were discovered in the 1970s. Researchers tried to make them into medicines, but they didn’t reach the brain well when injected and degraded quickly. Taking the enkephalin gene, which gives rise to proenkephalin and then enkephalin, researchers found that it could provide pain relief, especially in patients who didn’t respond to morphine. We showed that we could deliver enkephalin to the brain through a nose-to-brain route, making it a viable candidate for Envelta.

Image Credit: fizkes/Shutterstock.com
From a small molecule to addressing the big issue of the opioid crisis - what are your hopes for this treatment?
The opioid crisis, mainly in the U.S. but growing globally, is a major issue. Opioid drugs weren’t always controlled in supply, leading to widespread addiction. While opioids are effective painkillers, they have side effects like constipation, euphoria, and respiratory depression. We thought enkephalin, a molecule naturally secreted in the brain, could provide pain relief without these side effects. Animal studies haven’t shown reward-seeking behavior, giving us hope that it won’t cause euphoria in humans, and these specific receptors seem to be less problematic for respiratory depression.
We’re working on one formulation for eyedrops while our licensor develops another for painkillers. They’ve manufactured it and are now filling the delivery devices.
Now that you’re at this stage, what has the process taught you about drug discovery and delivery?
Scaling up production has been a major learning experience. Moving from milligrams to kilograms isn’t just a matter of scaling vessels and solvents—it involves waste management, space constraints, and other logistics. It took us about two years to scale from 500 milligrams to 100 grams and another year and a half to reach kilogram production.
During your talk, you emphasized the connection between discovery and delivery. How important is it for those involved in each to consider the other?
It’s crucial. Drug delivery scientists focus on making hard-to-deliver molecules accessible. Drug discovery scientists often adjust a molecule’s chemistry to improve solubility or permeability, but collaborating with drug delivery experts could help find packaging solutions without changing the chemistry.
You highlighted nanomedicine’s versatility in conditions like cancer and neurological diseases. What are your hopes for the future of this field?
The pandemic put nanoparticles in the spotlight for vaccine delivery. Nanotechnology in drug delivery has been around since the late 1970s, but it only gained widespread attention recently. Now, researchers are considering nanoparticles for a broader range of therapeutics, which is fantastic.
About Ijeoma Uchegbu
Ijeoma Uchegbu is Professor of Pharmaceutical Nanoscience at UCL, a fellow of the Academy of Medical Sciences, an honorary fellow of the Royal Society of Chemistry, a governor on the Wellcomemboard and Co-Founder and CSO of Nanomerics. She will also take up the position of President of Wolfson College, University of Cambridge later this year. Prof Uchegbu has served as Chair of the Academy of Pharmaceutical Sciences, Scientific Secretary of the Controlled Release Society and UCL Provost’s Envoy for Race Equality. Her pioneering work on the mechanisms of drug transport led to the discovery of transformational peptide nanoparticles that can be delivered across the blood brain barrier, namely enkephalin pain medicine candidate, Envelta™. She has been awarded various prizes for her work and is listed in Bloomsbury Publishing’s Who’s Who 2024.
She will also take up the position of President of Wolfson College, University of Cambridge later this year. Prof Uchegbu has served as Chair of the Academy of Pharmaceutical Sciences, Scientific Secretary of the Controlled Release Society and UCL Provost’s Envoy for Race Equality. Her pioneering work on the mechanisms of drug transport led to the discovery of transformational peptide nanoparticles that can be delivered across the blood brain barrier, namely enkephalin pain medicine candidate, Envelta™. She has been awarded various prizes for her work and is listed in Bloomsbury Publishing’s Who’s Who 2024.

 2 hours ago
2
2 hours ago
2













.png)

.png)
.png)
.png)












 English (US) ·
English (US) ·  Hindi (IN) ·
Hindi (IN) ·