Post-pandemic rebound in antibiotic consumption, especially in middle-income countries, raises concerns about antimicrobial resistance and global health challenges.
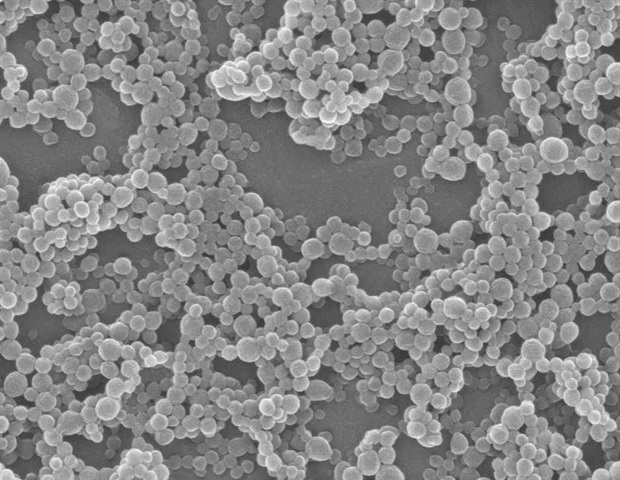
 Study: Global trends in antibiotic consumption during 2016–2023 and future projections through 2030. Image Credit: Saiful52/Shutterstock.com
Study: Global trends in antibiotic consumption during 2016–2023 and future projections through 2030. Image Credit: Saiful52/Shutterstock.com
In a recent study published in The Proceedings of the National Academy of Sciences, a group of researchers analyzed antibiotic consumption trends (2016-2023), impacts of coronavirus disease 2019 (COVID-19), and economic growth, and project future use to guide antimicrobial resistance policies.
Background
Antibiotic resistance is a pressing global health challenge, contributing to nearly 5 million deaths in 2019, with the highest mortality rates in low-income countries despite lower consumption.
Resistance arises from overuse in humans, agriculture, and animals and poor infection control. Antibiotic consumption rose by 65% between 2000 and 2015, driven by economic growth in: lower-middle-income countries (LMICs), while high-income countries (HICs) maintain higher per capita rates.
Over-reliance on antibiotics, particularly in need of improved sanitation, increases resistance. Surveillance of antibiotic use is critical for tailoring policies and addressing disparities. Further research is needed to link consumption trends with resistance and outcomes.
About the study
Data were retrieved for 67 countries using the IQVIA Medical Information Data Analysis System (MIDAS) database, which provides estimates of pharmaceutical drug sales. IQVIA MIDAS compiles monthly data from pharmacies and other outlets, categorizing consumption by retail and hospital sectors.
Antibiotic quantities were measured in kilograms of active ingredients and converted into defined daily doses (DDDs) using the World Health Organization (WHO) Anatomical Therapeutic Chemical Classification System (ATC/DDD). Hospital-sector antibiotics were assumed to be administered intravenously, while retail-sector antibiotics were considered orally administered.
DDD values for combination drugs were calculated by separating and analyzing individual molecules, and estimates were derived from additional sources for molecules lacking defined DDDs.
Population data from the World Bank and national governments were used to calculate consumption rates in DDDs per 1,000 inhabitants per day. Countries were grouped by 2023 World Bank income classifications: LMICs, upper-middle-income countries (UMICs), and HICs.
Antibiotics were further categorized using the WHO AWaRe framework (Access and Watch). Interrupted time series analyses (ITSAs) evaluated the impact of the COVID-19 pandemic on consumption, while global use projections to 2030 were generated using extrapolation and sensitivity analysis. Data cleaning and visualization were conducted using Stata, R, and Excel.
Study results
Between 2016 and 2023, total antibiotic consumption in the 67 countries with available data increased by 16.3%, rising from 29.5 to 34.3 billion DDDs. Over the same period, the average antibiotic consumption rate increased by 10.6%, from 13.7 to 15.2 DDDs per 1,000 inhabitants per day. Notable variations were observed across income groups as defined by the World Bank.
MICs, encompassing both LMICs and UMICs, saw an 18.6% increase in consumption rates compared to a 4.9% decrease in HICs. The COVID-19 pandemic had a marked impact, with consumption declining significantly in 2020, particularly in HICs (−17.8%), before rebounding in MICs.
The largest percentage increases in antibiotic consumption occurred in MICs, particularly in LMICs like Vietnam, where rates more than doubled, and in UMICs such as Thailand and Central America. By 2023, three LMICs and three UMICs ranked among the top 10 countries for antibiotic consumption, highlighting shifts in global patterns.
Conversely, the countries with the steepest declines during the pandemic included the Philippines and Malaysia. Recovery rates post-pandemic varied, with MICs experiencing rapid increases led by countries like Indonesia, Argentina, and India.
Antibiotic consumption also shifted by drug class. Broad-spectrum penicillins, cephalosporins, and macrolides remained the most consumed, though usage trends differed across income groups.
By the end of the study period, MICs surpassed HICs in macrolide and fluoroquinolone consumption rates, largely due to increases in LMICs. Consumption of "last-resort" antibiotics, such as carbapenems and oxazolidinones, rose sharply in MICs, indicating emerging resistance challenges.
Differences in Access and Watch antibiotic usage were evident. HICs consistently consumed more Access antibiotics, with their Access-to-Watch index increasing, while MICs consumed more Watch antibiotics, particularly in LMICs. By 2023, LMICs led in Watch consumption, reflecting disparities in stewardship practices.
Global antibiotic consumption in 2023, including estimates for missing data, reached 49.3 billion DDDs, or 17.0 DDDs per 1,000 inhabitants per day, marking a 20.9% increase in total use since 2016.
Projections suggest that, without policy changes, global consumption could rise by 52.3% by 2030, potentially reaching 75.1 billion DDDs, underscoring the urgent need for targeted interventions.
Conclusions
To summarize, between 2016 and 2023, global antibiotic consumption rose by 20.9%, slower than the 35.5% increase from 2008 to 2015, with a significant decline in 2020 due to the COVID-19 pandemic.
HICs saw the largest reductions, influenced by public health measures, while MICs rebounded rapidly post-pandemic, driven by economic growth and urbanization. MICs also saw rising use of last-resort antibiotics and fluoroquinolones, highlighting gaps in stewardship.
Addressing these trends requires stronger regulation, equitable access, and investment in preventive measures like sanitation, vaccination, and diagnostics, alongside global frameworks like WHO’s AWaRe to combat antimicrobial resistance effectively.
Journal reference:
-
E.Y. Klein, I. Impalli, S. Poleon, et al. (2024) Global trends in antibiotic consumption during 2016–2023 and future projections through 2030, Proc. Natl. Acad. Sci. doi:https://doi.org/10.1073/pnas.2411919121. https://www.pnas.org/doi/10.1073/pnas.2411919121

 1 day ago
1
1 day ago
1












.png)

.png)
.png)
.png)













 English (US) ·
English (US) ·  Hindi (IN) ·
Hindi (IN) ·